The National Suicide Prevention Trial was announced by the Australian Government in 2016. It was designed to gather evidence and further understanding of what strategies are most effective in preventing suicide at a local level and in at-risk populations. More specifically, its objective was to provide evidence of how an evidence-based multi-component systems approach to suicide prevention might best be undertaken within the Australian context and to identify new learnings in relation to suicide prevention in at-risk population groups including people who have attempted suicide or are considered at risk of suicide, Aboriginal and Torres Strait Islander peoples, young adult and middle-aged men, young people, and ex-Australian Defence Force (ADF) members, and lesbian, gay, bisexual, transgender and intersex (LGBTI) people.
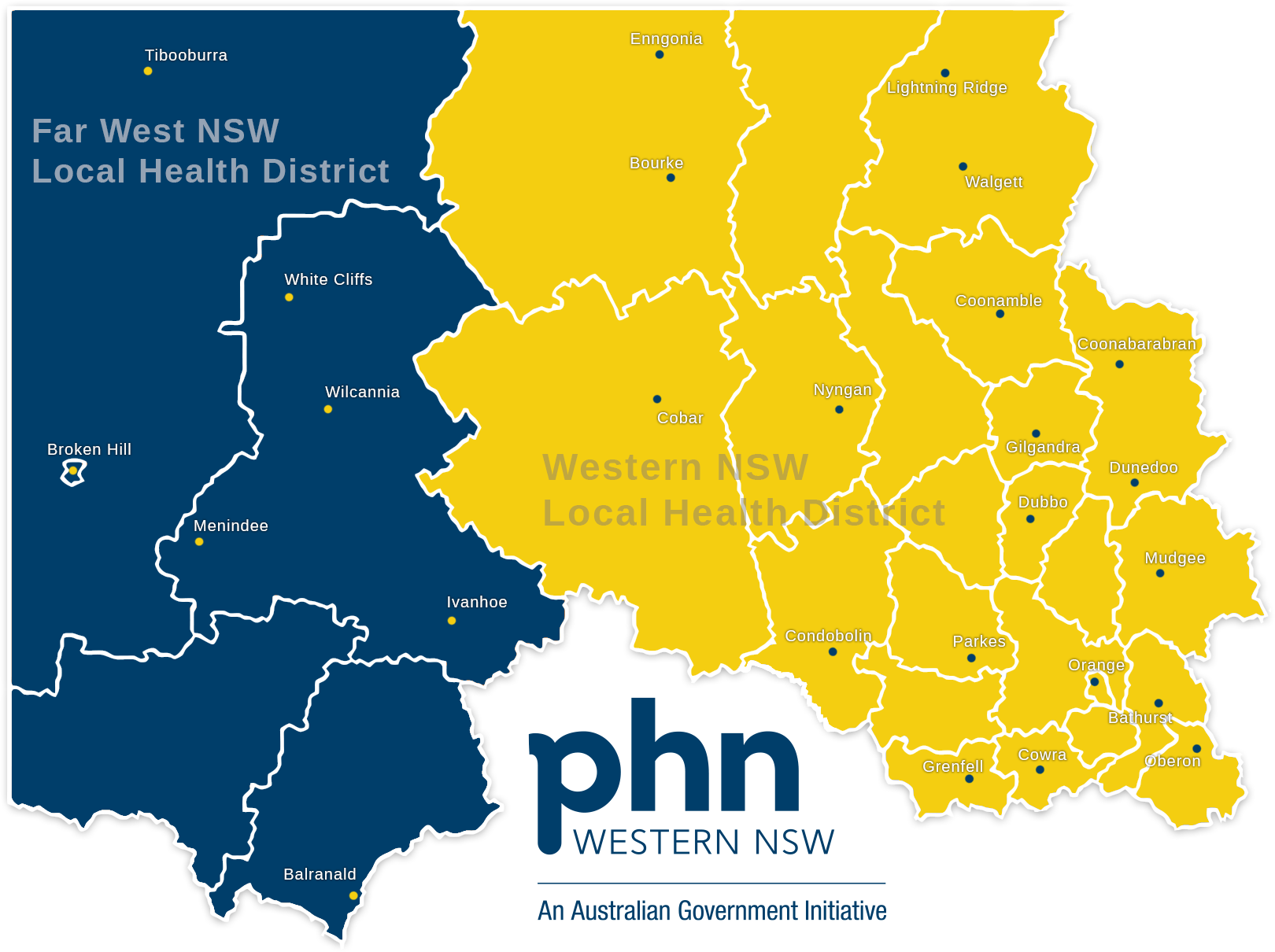
Twelve Trial Sites were selected (Townsville, Central Queensland, Brisbane North, North Coast NSW, Western NSW, Northwest Melbourne, Tasmania, Country South Australia, Perth South, Mid-west Western Australia, the Kimberley, and Darwin), managed by 11 Primary Health Networks (PHNs).
PHNs are key to the successful delivery of the Australian Government’s approach to suicide prevention. Thirty-one PHNs were established in July 2015 following a review of their predecessors, Medicare Locals. The objective of PHNs is to ‘increase the efficiency and effectiveness of medical services for patients, particularly those at risk of poor health outcomes, and to improve coordination of care to ensure patients receive the right care in the right place at the right time’. PHNs are
responsible for the planning and commissioning of primary mental health care services, including suicide prevention activities, via what is known as the Primary Mental Health Care Activity.
PHNs made extensive efforts to plan suicide prevention services and activities that responded to local needs. Most relevant, was the need to build capacity by providing community stakeholders with foundational understanding of evidence-based and systems approaches facilitated full community participation in the Trial. More specifically, workforce capacity building in terms of recruiting and supporting a dedicated suicide prevention coordinator role was also crucial to maintaining engagement of stakeholders and momentum in the planning process. Through such, the Workforce Capacity Building Program was born.
Trial Sites undertook an extensive planning process and then commissioned a range of evidence-based, evidence-informed and innovative interventions guided by multi-component models including the Lifespan and Alliance Against Depression frameworks. Sites focusing on suicide prevention for Aboriginal and Torres Strait Islander peoples drew on the Aboriginal and Torres Strait Islander Suicide Prevention Evaluation Project (ATSISPEP) findings and principles. The Black Dog Institute was commissioned by the Department of Health to provide support to the PHNs in relation to planning, and the selection and implementation of evidence-based strategies.
Four Trial Sites commissioned aftercare services for people who had attempted suicide or were experiencing a suicidal crisis, and all Trial sites commissioned a range of community-based activities. The majority of those activities were either awareness raising and engagement activities or capacity building. These included providing training to community members, frontline workers and members of the health and allied health workforce on suicide prevention or offering mental health first aid training. Other activities involved providing information or activities for particular at-risk groups or individuals, cultural strengthening activities for Aboriginal and Torres Strait Islander peoples and communities, and the development of information resources and care pathways. All Trial Sites also undertook activities aimed at increasing integration and coordination among existing suicide prevention services and activity providers in the sector.